The use of the computer-aided detection (CAD) system, Magentiq-COLO (Magentiq Eye), led to an absolute increase of 0.19 (relative increase, 37%) in adenomas per colonoscopy (APC) and an absolute increase of 7% (relative increase, 23%) in the adenoma detection rate (ADR). In the tandem study, the adenoma miss rate (AMR) was 17% lower with CAD, reflecting a relative decrease of 47% over conventional colonoscopy, according to the investigators, led by Michiel H.J. Maas, MD, of Radboud University Medical Centre, in the Netherlands (Lancet Digital Health 2024;6[3]:E157-E165).
Dr. Maas and his co-investigators noted that the findings are generally in sync with other studies of CAD systems (Gastroenterology 2022; 163[3]:732-741; Clin Gastroenterol Hepatol 2022;20[7]:1499-1507; Lancet Gastroenterol Hepatol 2023;8[8]:726-734; Gut 2022;71[4]: 757-765; Gastrointest Endosc 2021;93[1]:77-85).
Co-investigator Suzanne Lewis, MD, an associate professor of medicine at Columbia University Vagelos College of Physicians and Surgeons, in New York City, told Gastroenterology & Endoscopy News that the advantages of CAD colonoscopy related to APC and AMR came “without an increase in the resection of nonadenomatous lesions.”
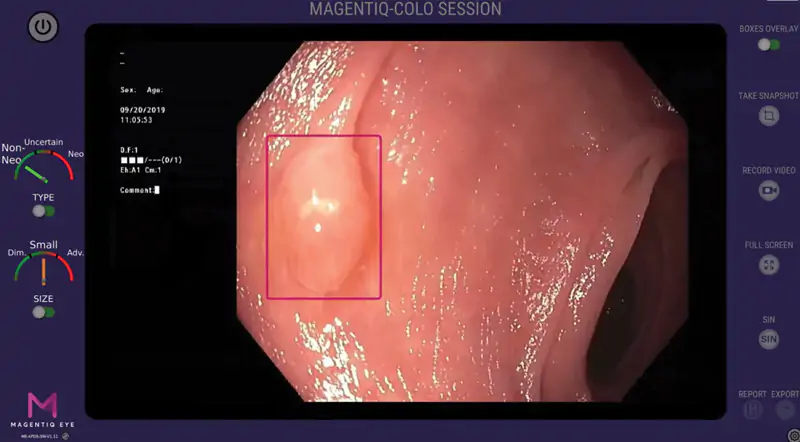
The randomized, 10-center study compared outcomes with CAD and conventional colonoscopy in patients undergoing colonoscopy screening or surveillance who were not referred for a positive fecal immunochemical test. The final intent-to-treat analysis included 916 patients—449 undergoing CAD and 467 having conventional colonoscopy. For the tandem substudy, 61 underwent CAD first and 66 had conventional colonoscopy first.
CAD Improves Most End Points
The use of CAD improved the co-primary end point of APC during the first examination. For CAD and conventional colonoscopies, the number of total adenomas detected per colonoscopy was 314 of 449 versus 238 of 467, respectively, translating to a 37% relative increase in APC with CAD. In a post hoc regression analysis, a significant 56% increase in APC was achieved (P=0.005). For the second co-primary end point, adenomas per extraction (APE) during the first exam, CAD was noninferior to conventional colonoscopy, but mean per-patient APE was higher with CAD (0.27 vs. 0.31).
For the secondary end point of ADR, CAD was also superior, and CAD detected numerically more sessile serrated lesions (SSLs), but the difference was not statistically significant.
In the tandem study, endoscopists using CAD missed significantly fewer adenomas, with 11 detected in the subsequent conventional examination compared with 29 detected by subsequent CAD after conventional colonoscopy.
For the 19% of adenomas still missed with CAD first, post hoc video analysis showed that they were mostly not visible in the visual field and, thus, could not have been detected by CAD. This observation suggests that the combination of CAD and a mucosal exposure technique might further improve detection, the investigators noted.
Details of these and other outcomes for the modified intent-to-treat population, by study group, are shown in the Table.
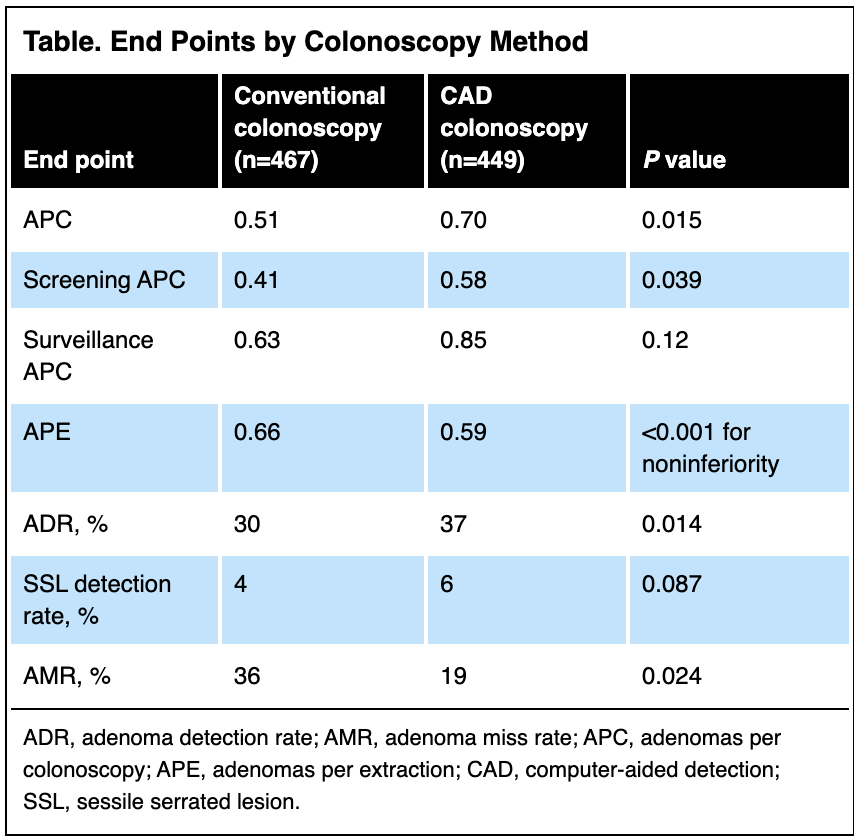
The use of CAD did not increase mean withdrawal time, which was 6.5 minutes in each arm, without interventions, in the first exam and six minutes in each after the second exam.
Jeremy R. Glissen Brown, MD, MSc, an assistant professor of medicine at Duke University School of Medicine, in Durham, N.C., said the study adds to an “ever-growing body” of trial data showing that CAD can improve most conventional colonoscopy quality metrics. “This study is impressive in that it is one of the largest multinational CAD studies to date and serves as the data foundation for the recent FDA approval of the Magentiq-COLO system in the United States,” he said. He also lauded the investigators for conducting a nested tandem colonoscopy study within the trial and a post hoc video analysis to characterize the missed lesions.
“There was also no significant increase in procedure time or withdrawal time, though one of the study’s limitations is that the withdrawal time in both groups was on the lower end of the spectrum. There was also not a statistically significant increase in sessile serrated lesion detection in the CAD group versus controls,” he said, although he noted that “there has been some heterogeneity here, in general, between trials/systems.”
Drs. Glissen Brown and Lewis agreed about the need to examine the impact of CAD on mid- and long-term health outcomes, to assess the willingness of physicians to use CAD in their practices, and to determine how best to integrate it into health systems.
The article was originally published in gastroendonews.com

