

When analyzing the financial benefits, it’s important to explain the vast difference between Europe and the US, in the percentage of the population undergoing colonoscopy, and in the structure of the healthcare systems.
US: Private healthcare, clear monetary incentive
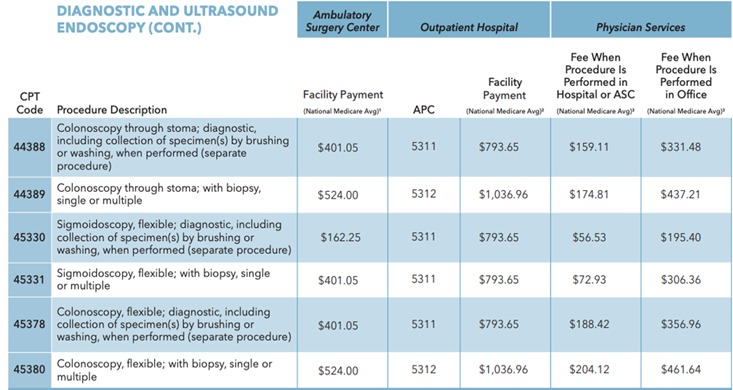
In the US, colonoscopy is covered by healthcare insurance providers, and is recommended to patients over the age of 45. Payment by insurer is calculated according to a price list by CPT codes, which takes into account different factors, for example if the procedure included resections or not. According to this model, for every procedure in which there was a polyp resection or biopsy, the outpatient hospital earns around US $240 in additional fees. It is easy to see how an increase in Adenoma Detection Rate (ADR) and Polyp Detection Rate (PDR) are translated into income. Moreover, patients with detected adenomas are required to perform colonoscopy every 1-3 years instead of every 5 or 10, and finally, prevention is always cheaper than treatment.
And last, but definitely not least, an increase in ADR leads to a decrease in Colorectal Cancer (CRC) (Corley D.A., Jensen C.D., Marks A.R., et al. Adenoma detection rate and risk of colorectal cancer and death, N Engl J Med. 2014; 370: 1298-1306.), and therefore AI systems, which increase ADR have the potential to lead to save cost associated with of CRC treatment.
In conclusion, in the US (and other markets), improved performance presents a huge financial incentive to health insurers and HMO but also benefits the bottom line of the individual colonoscopist.
Europe: Public healthcare, lower rate colonoscopies per population
In comparison, most European countries have a public healthcare system, Here, Fecal Occult Blood Test (FOBT) is still the most common method of screening, while colonoscopy is available only in cases where blood in stool is detected. If we look at Italy as an example, FOBT results send only 1-2% of the tested population to perform colonoscopy screening, but in reality, 5% of the FOBT tested population exhibits early signs of colon cancer. Netherlands and Spain show similar data. There is growing realization in Europe that FOBT is not enough, and in the past 10 years we are seeing a consistent increase in the number of colonoscopies performed in most European countries, but it is still only about half of the colonoscopies done annually in the US. To date, Germany is the only country in Europe where the public healthcare system covers colonoscopy screening for anyone above 50 but we can expect additional countries to follow this example.
“Public systems investing in mass screening are concerned with the quality of colonoscopy,” says Jen Kees Dunning, a Netherlands based healthcare consultant and senior advisor to the MAGENTIQ EYE. He explains that because colonoscopy has not been done on a large scale until now, there’s a shortage of professionals to support the mass screening goal. Dunning estimates that the financial burden of transitioning into mass screening is about 10 years, but with AI in the game, it can be cut to between 2-6 years depending on the specific market.
Here too, we are looking at additional savings stemming from the connection between increased ADR and lowering the risk of CRC.
Leveling the playing field
“For the medical community, AI allows gastroenterology residents to develop their skills quickly, and bridges the experience gap between physicians with less colonoscopy experience to top tier experts,” says Dr. Harold Jacob. MD, Director of Gastrointestinal Endoscopy at Hadassah University Medical Center.
Using AI aided colonoscopy in training, and for sharpening professional skills, provides an additional financial incentive as it allows new doctors to start performing these procedures with less supervision than before. This is especially important in places where the demand for colonoscopy is high.